HL7 Integration: How to Build Interoperability Interface for Your Healthcare Systems

How does HL7 work and how should you implement a healthcare integration engine? In this article, we’ll discuss everything there is to know about HL7 standard integration and other interoperability development services for healthcare applications and medical IT projects.
Health Level 7 (HL7®) Standards were designed to allow different healthcare organizations to exchange clinical and administrative data between their computer systems easily, consistently, and without costly technical limitations. Collaborating with an EHR software development company can ensure seamless integration of HL7 standards into your healthcare systems, enhancing interoperability and data exchange efficiency. The most popular up-to-date HL7 medical system interoperability protocols include HL7 V2, V3, and FHIR.
| ? NOTE: If you seek best practices for integrating HL7 interfaces and formatting methods into your medical software projects, please contact us for a free consultation. TATEEDA GLOBAL can help you with required HL7 integration services and building a healthcare integration engine in multiple contexts, including project-based HL7 team augmentation and full-cycle medical software project development with custom Azure cloud solutions, IoT, and other technologies. |
HL7 offers well-documented standards recognized and defined by ISO/IEC, an international non-profit standards organization. The HL7 standard was accepted after many years of continuous efforts and experiments aimed at developing a common data exchange method to bridge disparate healthcare IT systems across myriad American hospitals, medical centers, insurance companies, and other institutions.
Before we talk about the technical and business aspects of HL7 integration in healthcare tech environments, let’s learn the basic facts about this standard…
What is the latest HL7 protocol, and what is the most popular one?
Although HL7 has been considered a de-facto standard for some time now, HL7 version 3 has become a formal standard accredited by ANSI (American National Standards Institute.) ANSI-approved HL7 version 3 consists of a set of mandatory and optional specifications that describe the system interfaces and data structures required for electronic healthcare information exchange.
Nowadays, 95% of healthcare organizations in the United States adhere to HL7 v2 interface rules and formats. Additionally, the HL7 integration standard is the most widely adopted health information technology (HIT) integration standard in the world.

Do You Want to Integrate
HL7 Interoperability?
Since 2013, our health-tech team has been developing experience in HIPAA-compliant solutions, including HL7 FHIR for data exchange.
What is the HL7 standard from a technical perspective?
The Health Level 7 international standard is a set of messaging rules that allow software and other health technology systems to communicate with each other through a component called the HL7 integration engine. Messages follow HL7 specifications. They are ASCII-formatted, and must include several crucial segments:
- Message header (MSH): This segment contains the name of the sender, the name of the receiver, the time the message was created, and other important signature data.
- Patient identification (PID): This segment includes patient demographic, PHI, SSN number, marital status details, and more.
- Diagnosis (DG1): This segment includes multiple fields to describe patient diagnosis parameters.
Other frequently used segments in HL7 messages include…
- Event type (EVN)
- Guarantor (GT1)
- Insurance (IN1)
- Next of kin/associated parties (NK1)
- Notes and comments (NTE)
- Observation request (OBR)
- Observation result (OBX)
- Common order (ORC)
- Financial transaction (FT1)
Each segment of an HL7 message consists of specific data fields used to specify and communicate all necessary details, which must be correctly marked with specific symbols (delimiters) so they can be easily interpreted by the receiving systems.
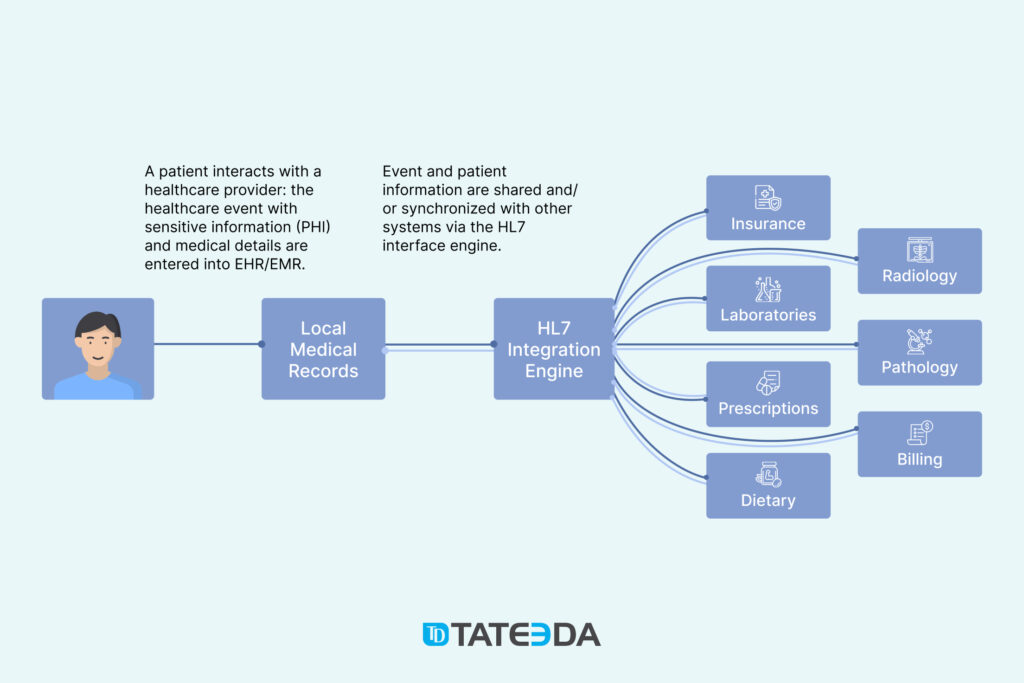
How is HL7 used in healthcare?
HL7 mandatory guidelines allow hiring dedicated software developers to integrate a medical application with other applications that follow the same standards to make sure they “speak the same language” in the process of data exchange. They are used to create new healthcare software products and establish efficient machine communications between existing solutions in hospitals and other medical facilities.
In addition, HL7 creates a common framework for operating medical data, which then allows software systems from different vendors to update and exchange sensitive information in a HIPAA-compliant manner (secure, protected, and manageable.) HL7 provides standardization and codification for different healthcare process operations and occurrences specific to hospital workflows. These events and data transactions include:
- Patient admission and discharge notifications
- Patient transfers and status changes
- Clinical trial and medical study information
- Disease and/or allergy status updates
- Medical supervisor detail updates
- Lab results and master file transfers
- Pharmacy and diet orders.
Why integrate HL7 standards in healthcare operations?
- The main reason is desired cost-efficiency. According to existing estimates, the propagation of HL7-based interoperability techniques leads to an annual reduction in overall healthcare costs of around $30 billion, thanks to the benefits of medical system unification. This allows elimination of excessive IT effort formerly dedicated to building unique digital solutions for each individual healthcare client.
- Unification of communication: Suppose you want your application to be smoothly integrated into a common healthcare IT landscape to share and synchronize electronic records. In that case, HL7 is the right mechanism for enhanced medical IT system interoperability. It’s a well-designed and reliable solution.
- Comprehensive instrument: Thanks to HL7 interface integration, developers don’t have to invent and build expensive unique interfaces to interconnect two or more medical systems from scratch. Instead, they can reduce development costs by implementing a readily available, commonly recognized set of communication rules suggested by HL7 protocols.
Is there an alternative to HL7?
While HL7 guidelines have been a standard in healthcare for several decades, other standards are being developed for this purpose. The most prominent of these are DICOM and CDA (the latter is a domain of HL7 V3). Other healthcare IT experts have pointed out that there is a need for open-source data exchange technologies, and have identified FHIR and CDISC as promising new alternatives to consider.
Learn more: ➡️ How to Move to the Cloud for Healthcare Companies & Organizations
What is the difference between FHIR and HL7 version 2/3?
Despite the fact that FHIR (the current version is FHIR release 4) and HL7 (V2 and V3) are all sponsored and managed by the same HL7 organization, they still feature significant differences. FHIR is a newer standard that employs RESTful services and supports a variety of open web formats like XML, JSON, and RDF. At the same time, HL7 maintains only documents in XML format. Since FHIR stems from previous standards (HL7 CDA, V2, and V3), it shares similar functionalities but offers far more versatile and convenient capabilities, embracing a broader spectrum of data formats and API integrations.
| HL7 V2 | HL7 V3 | HL7 CDA | FHIR | |
| Format | Structured Message | Structured Message | Clinical Document Architecture (XML-based markup) | XML/JSON and API integrations: RESTful web services |
| How it is used | Patient record and medical data exchange | Patient record and medical data exchange | Clinical document exchange and management | Universal healthcare data exchange covering medical record updates, connected application functionalities, medical IoT devices, and smart wearables |
| Platforms | EMR, EHR, HIS, LIS (LIMS) and more | EMR, EHR, HIS, LIS (LIMS), and more | EMR, EHR, HIS, LIS (LIMS), and more | EMR, EHR, HIS, LIMS, mobile apps, IoT, medical devices |
Learn more: ➡️ Custom EHR & EMR Software Development Services

| ? Are you interested in hiring HL7 integration specialists and outsourced services for your healthcare IT interoperability project? If you want to discuss HL7 standard integration for your medical software project, including HL7 FHIR implementation services in developing a cross-platform healthcare management system, please book a free consultation with our experienced healthcare IT engineers. Tell us more about your objectives and expectations, so we can provide you with personalized HL7 integration services including deeper consulting and a free project estimate: ? |

Slava Khristich
Healthtech CTO
Based in San Diego, Slava knows how to design an efficient software solution for healthcare, including IoT, Cloud, and embedded systems.
Table of Contents
The Core Tasks and Features of HL7 Integration in Healthcare IT Products
The highest tier of HL7 objectives and healthcare requirements include the following…
- Patient-centric healthcare principles
- Data-driven medical practices
- Coordinated patient care approach
- Value-based, ethical decision-making
- High patient service quality and expectations
- Compliance with specific data-privacy policies
- Enhanced practices for processing ever-growing volumes of data
- Technical preparedness for automated clinical decision-making
- Availability of medical data mining and machine-aided data processing
- Intensified demand for telehealth services and applications.

Please note that some of these are directly supported by specific regulations in the United States: Policies and Technology for Interoperability and Burden Reduction.
| HL7 integration ensures configurability of medical system conglomerates. The above-mentioned aspects require medical systems to have high acceptance of unified information exchange methods so medical data flows can be redirected, organized, and consolidated quickly, in a very flexible manner. HL7 and FHIR satisfy modern requirements and help developers avoid reinventing the wheel for every new client while seamlessly integrating different systems. |
Business Functionalities Covered by HL7 Specifications
Some of the most popular medical and business functionalities covered by HL7-enhanced healthcare software and instrumental integrations include…
- All types of EHR & EMR features and operations
- Billing and reimbursements
- Medical record maintenance and updates
- Telehealth system services and applications
- Patient administration in clinical workflows
- Pharmacy and laboratory workflows
- Immunization and allergy statuses
- Insurance claim management
- Clinical reporting and asset management
- Patient and physician appointment scheduling.
Learn more: ➡️ The Major Healthcare Technology Trends
How to Configure Interoperability in Medical Systems: The Four Main Tasks of HL7 Integrators
General tech tasks to be executed under HL7 interface integration include…
- Identification of the source medical software system(s), which transmits the data to a target system.
- Identification of the target medical IT system(s) receiving data from a source system.
- Mapping of data elements in an HL7-formatted manner and configuring specific programmatic interfaces and engines to transmit messages between the source and target systems.
- Transferring data between the two systems: keeping data accurate in the process of transmission; keeping data correctly coded by the source system and decoded at the endpoint according to predefined business and technical rules.
Components of HL7 Integration: EDI, Coding, Translation of Messages, and More
The name Health Level Seven refers to the highest (7th) level (called application layer) of the OSI communication model, which describes cross-application relations between two networked PCs. The HL7 model does not set any strict requirements for the way HL7 messages are transmitted; however, the most popular transport methods include the following application-level protocols:
- File Transfer Protocol (FTP)
- Simple Object Access Protocol (SOAP)
- Simple Mail Transfer Protocol (SMTP)
The process of HL7 configuration and implementation involves many functions and aspects referring to…
HL7 Electronic Data Interchange (EDI) – the most common task performed by HL7 integrators, allowing the exchange of structured documents in a way that both parties can understand. Aspects to be considered by developers in the EDI context include…
- The specifics of the device(s) and networks used to transmit the data: The OSI levels beyond the Application Layer must be taken into account, too.
- The software solution or HL7 engine that translates data into a standardized electronic data exchange format in accordance with business rules.
- The technical parameters of the communication channel existing between the sender and the recipient.
- Users who are permitted to send and receive medical information: data transmission initiation rules, user authorization options, and more.
HL7 Clinical Document Architecture (CDA) – clinical documents (such as a progress medical note or patient billing summary) transmitted with the help of HL7 standards and guidelines must use specific document markup structure and semantics. A CDA document employs XML (Extensible Markup Language) and can incorporate message text, images, and multimedia files.
HL7 Message Translation – the process and algorithm of converting medical messages from one data format to another while keeping value and meaning intact; often used for interconnecting legacy systems or applications employing different standards when their output must be formatted and deciphered with the HL7 engine. Learn more: ➡️ Legacy Systems in Healthcare: How to Upgrade Outdated Software Solutions.
Business Rules – local business logic that is not implicit in HL7 specifications but must be applied when creating a message or processing a received message in a specific operational context. This requires individualized attention and deeper customization efforts from medical software integrators.
HL7 Message Implementation Guidelines – HL7 offers sufficient flexibility to create custom messaging structures without causing serious system errors, according to local guidelines accepted by a wide range of medical industry organizations. The HL7 Reference Information Model (RIM) applies static healthcare terminology to standard healthcare workflows, but there is always enough room for negotiable interface improvements and changes, such as…
- Local variations of data interchange rules, including optional HL7 message structures, groups, segments, composites (fields), and more.
- The ability to use different protocols and coding rules for HL7 messaging between healthcare IT systems.
- Additional system functionalities and local variations of HL7 implementation available as required to handle individual client situations and needs.
HL7 Engine Development – One of the main HL7 data integration tasks is the development of custom interface engines, which are software components intended to automatically filter, regulate, and route data flow between applications. These software solutions embrace the two-layered nature of the HL7 standard, covering both medical system data specifications and message specifications.

Do You Need to Build an HL7 Integration Engine?
Our engineers help you interconnect several medical systems so they seamlessly exchange sensitive data according to HL7 rules.
How to Build an HL7 Interface?
Creating an HL7 interface involves a series of steps:
- Establish Objectives: Start by defining your goals for the HL7 interface, specifying the data to be exchanged and the systems involved.
- Choose Integration Solution: Select the right HL7 interface development solution that suits your requirements, whether it’s middleware, an interface engine, or custom development.
- HL7 Version: Identify the HL7 version you will work with; be it HL7 v2 or HL7 v3, as each has its unique standards and formats.
- Data Mapping: Map the data elements between the source and target systems, aligning data fields and establishing transformation rules.
- Message Creation: Craft HL7 messages based on the mapped data, ensuring adherence to the HL7 standard for your chosen version.
- Testing: Rigorously test the interface to guarantee accurate and secure data transmission, identifying and addressing any issues.
- Error Handling: Develop a reliable error-handling mechanism to manage potential issues that might arise during data exchange.
- Documentation: Maintain comprehensive documentation covering the HL7 interface development, including message formats, transformation rules, and troubleshooting procedures.
- Compliance: Ensure that your HL7 interface complies with pertinent healthcare industry regulations and standards.
- Training: Provide training to the staff responsible for operating and maintaining the interface, ensuring they have a firm grasp of the system and its troubleshooting protocols.
- Monitoring and Maintenance: Continually monitor the interface’s performance and address any emerging issues promptly. Regularly update the interface to accommodate shifts in data requirements or HL7 standards.
The process of building an HL7 interface demands planning, meticulous attention to detail, and a profound understanding of data exchange needs within the healthcare domain.
| ? If you require HL7 integration services to interconnect hospitals, health data-management systems, or any other clinical or non-clinical applications via secure XML or JSON transmission and/or other HL7-specified methods, we are here to help you with development and quality assurance. TATEEDA GLOBAL offers HL7 integration expertise and assistance in the context of medical programming projects including custom HL7 interface development: ? |
Custom Healthcare Solutions
See how we can engineer healthcare software, validate your ideas, and manage project costs for you.
Why Healthcare Organizations Need an HL7 Integration
As we learned from the previous paragraphs, system compliance with HL7 standards simplifies and enhances the data exchange process. Moreover, the implementation of HL7 standards helps reduce costs and improve the quality of healthcare with smooth interoperability between a range of clinical, financial, and administrative systems: EHRs, HIS, IDNs, RISs, RISCs, CPOEs, and other healthcare software applications. The standard enables information exchange between diverse software products to manage:
- Hospital medical records systems (HIS)
- Healthcare enterprise resource planning system (ERP)
- Emergency medical services (EMS)
- Laboratory information systems (LIS)
- Radiology information systems (RIS)
- Remote ECG-monitoring software
- Immunization information systems (IIS)
- Healthcare staff payroll software
- Pharmacy management systems (PMS)
- Patient electronic data capture solution
- Any other systems used for collecting or storing health care data.
The Major Benefits of HL7 Standard Integration
- Provides a common language for all of your EMR and EHR systems
- Allows you to seamlessly exchange clinical data with other practices/providers
- Increases the speed of data exchange across medical software systems
- Supports effective workflow automation
- Reduces the risk of data loss or corruption
- Helps to ensure that only authorized persons have access to clinical data.
How Hospitals Benefit from HL7 Integration
HL7 hospital integration helps hospitals streamline the process of exchanging patient data in the context of lab results exchange, clinical decision support systems, referrals, orders, and patient billing. If you want to develop or upgrade a hospital information management system, feel free to contact us.
Thanks to HL7 integration strategies for hospitals, medical professionals can reduce the time needed to transfer and manage information. This leads to better treatment analytics and improved patient outcomes. In addition, hospitals can gain significant advantages by implementing HL7 standards, including…
- Convenient, secure, individualized medical data access portals for physicians, nurses, and healthcare specialists.
- Better coordination of clinical, administrative, and financial transactions across multiple medical IT systems, hospital departments, and healthcare process stakeholders.
- Seamless migration and rapid propagation of files across multiple permissioned spaces. Examples include lab results, radiology images, X-rays, and other medical records generated by different healthcare software programs.
- Swift, accurate import and export of patient records between different EHR and EMR systems.
- Wide interoperability between hospital systems under the terms of inter-hospital collaborative efforts.
- Smooth data sharing between different hospital departments and clinicians.
- Prevention of duplicate data entries and minimize human error, misinterpretation, and uncertainty.
- Fulfillment of HIPAA requirements by providing patients with better online access to their medical records and histories via patient portal development.
- Facilitation of data analysis via Big Data solutions.
- Efficient distribution of hospital information and reports to government regulators and agencies.
Benefits of HL7 Integration for Health Insurance Providers
- HL7 integration enables insurers to receive real-time patient information from various sources, including hospitals, clinics, and laboratories.
- This allows them to make more informed decisions about coverage and claims.
- HL7 integration also provides a complete picture of patient health, which can help improve coordination of care among different providers.
- Finally, HL7 integration helps insurers save money by reducing the need for manual data entry and improving claim-processing accuracy.
HL7 Integration Challenges You May Face
Let’s consider several issues HL7 standard integrators can face when working with medical systems and health-tech interoperability development…
Lack of HL7 Integration Expertise
It’s essential that IT specialists possess prior experience in implementing Hl7-specified interoperability technologies. This is important because healthcare IT solutions incorporate numerous modules and applications that may be difficult to standardize and interconnect. Perfect knowledge of HL7 specifications and the ability to improvise are prerequisites for success.
The Lack of Skilled Medical System Engineers
Unfortunately, the IT market doesn’t offer a sufficient number of skilled resources to provide healthcare companies with unlimited HL7 implementation consulting and services. Some of the standards offered by this group (like FHIR) are relatively new, while others have a wide variety of versions and local implementations. A skilled medical software engineer can implement HL7-based interoperability within a reasonable time frame in terms of scope and costs.
HL7 Protocol Variations
HL7 organization maintains numerous standards and versions, including FHIR and HL7 V2/3 plus auxiliary documentation.
When it comes to setting interoperability between systems using different protocols and versions, the process requires that HL7 integrators know the specifics of each system and are able to design a programmatic connector converting formats between applications.
Otherwise, it may take too much time to learn HL7 documentation and comply with all of its nuances and mismatches.
| If you want to find a reliable medical IT partner for HL7 or FHIR integration, consider TATEEDA GLOBAL. We have extensive experience working with many businesses within the American healthcare industry. We offer custom IoT solutions and biotechnology application development services, and we can provide exemplary use cases involving the integration of the HL7 interface in our partners’ software products. Please learn more from our portfolio: ? |
Delivered Healthcare Software Portfolio
The leading American healthcare companies benefit from working with us.
Using API Approach for HL7 Integration
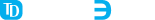
Modern flexibility to HL7 integration is ensured by the FHIR protocol that supports APIs. Thanks to a common set of APIs, developers can avoid building special interfaces and engines that deal with each system’s specifics, instead leveraging modern web technologies like HTTPS, REST, XML, JSON, and ATOM to connect applications like EHRs with third-party solutions, including custom patient portals and telemedicine apps.
Thanks to the RESTful approach, HL7 FHIR offers more room for system customization and encourages a seamless interoperability and communication model for multi-modular healthcare IT solutions. It’s even possible to accomplish the integration of FHIR interfaces in a single day. That’s because of the fast and easy implementation model it offers.
| Interested in healthcare integration engine development outsourcing services? If you want to develop custom patient claim-management and billing software, tailored hospital information-management software, custom medical staff management systems, and/or a telehealth application with interoperability features, we can help you design medical software architecture and implement an EHR/EMR HL7 interface solution matching your organization’s specifics. TATEEDA GLOBAL offers skilled software development outsourcing for American and global clients. Our team of senior nearshore developers, creative UI designers, experienced QA engineers, and skilled project managers are ready to guide you through the process of building HIPAA-compliant software. |
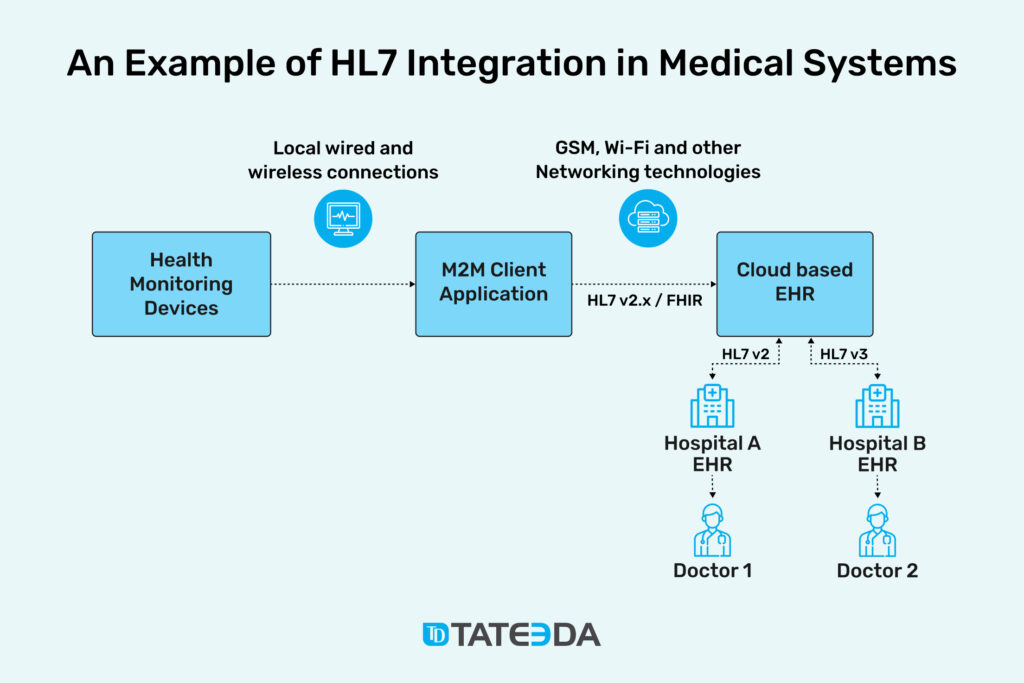
Practical Examples of HL7 Integrations in Medical Systems
Since HL7 integration enables automated data exchange between several healthcare applications or systems, it helps remove the administrative burden from nurses, medical officers, and other healthcare staff. All medical data exchange processes can now run smoothly without human intervention or supervision.
HL7 Interface Examples: Comparing FHIR vs. HL7 v2 Interface Message Formats and Versions
Here’s a simplified illustration of an HL7 v2 system message designed to facilitate the updating of patient demographic data between Electronic Medical Record (EMR) systems. It’s essential to note that HL7 messages can be highly intricate and tailored to specific needs, so the example provided here serves as a fundamental representation:

Within this instance:
- The MSH (Message Header) segment conveys vital message details, encompassing particulars about the systems involved in message exchange and associated timestamps.
- The EVN (Event Type) segment delineates the nature of the event, denoted as “A08” for a patient information update, along with the corresponding timestamp.
- The PID (Patient Identification) segment houses a repository of patient demographic information, encompassing details such as name, date of birth, gender, address, contact numbers, and additional particulars.
- The PV1 (Patient Visit) segment delivers insights into the patient’s visit, comprising information regarding the location and the medical personnel overseeing the visit.
HL7 FHIR (Fast Healthcare Interoperability Resources) messages introduce a higher level of complexity compared to traditional HL7 v2 messages, employing a format rooted in modern web standards. Here’s a basic model of an HL7 FHIR message designed for the purpose of updating patient demographic information:

Within this HL7 FHIR message instance:
- The message is structured in JSON format, a prevalent choice for FHIR messages.
- It adopts the FHIR Bundle resource type to encapsulate the entire message’s content.
- The central resource type is “Patient,” housing an array of patient demographic specifics, including but not limited to name, date of birth, gender, address, and contact particulars.
- Each element is portrayed as a distinct JSON object, featuring specific attributes in line with the FHIR standard.
It’s essential to acknowledge that this serves as a basic representation, as real-world HL7 FHIR messages can encompass a more extensive array of resources and particulars to accommodate the precise data requirements when facilitating information exchange between Electronic Medical Record (EMR) systems.
This requires a deeply individualized approach and custom services for the configuration of HL7 parameters and capabilities, including…
HL7 Configuration for Enhanced Laboratory Result Workflows
With FHIR or other interoperability standards specified by HL7, it’s easier to automate and consolidate the flow of lab results from various medical systems: for example, local department-based software that produces and stores multifaceted information.
With HL7 standards, it’s possible to…
- Keep laboratory records in sync across different systems and facilities, consolidating data from multiple sources such as radiology departments and pathology labs within EHR/EMR and patient portal solutions.
- Create, update, and share files such as diagnostic readings and conclusions through patient portals and other outlets for electronic results.
- Make sure all medical information is represented as accurately as possible when reviewed by physicians or healthcare process stakeholders via individualized interfaces and custom dashboards in mobile and web applications.
HL7 Connection between ERs and Other Healthcare Facilities
Emergency rooms capture crucial medical data like patient medical history, objective control of vital signs, X-rays, and more.
- Store medical files in one system, then immediately transmit or share data objects electronically with other systems as required by business and healthcare protocols.
- Ultimately, store all data in patient records (EHR). This allows you to share documents with other medical practitioners and allows physicians to view records at their convenience.
- Let medical professionals view lab results on the same screen where they enter orders and prescriptions for additional tests and/or procedures, thus reducing the likelihood of errors and shortening wait times for patients.
Build Complex Cross-platform Systems with HL7 Interfaces
When you integrate HL7 data from the EHR system into other clinical or nonclinical systems and vice-versa, you can assemble a truly powerful medical IT conglomerate that consolidates multiple functionalities and data flows with the following functionalities:…
- Receive complete medical history and access medical files of incoming patients for hospitals and emergencies
- Build shared knowledge bases and data access points for a variety of purposes.
- Medical CRM solutions for tracking patient satisfaction and feedback
- Doctor’s appointment schedulers and notifications for planning patient visits online
- Healthcare staff shift planners and medical procedure and task-management tools for physicians, surgeons, and nurses
- Cross-hospital collaboration in terms of patient health information exchange and synchronization
- Big Data analytics and other complex solutions.
HL7 Integration Procedure: Phases Required to Accomplish an HL7 Project
Here is a short example of how HL7 mandatory requirements for interface development and interconnectivity in medical systems can be executed and integrated into medical organizations…
Phase #1: Audit the Current IT Environment and Plan the HL7 Interface or Engine Structure
- Identify the systems to be integrated with each other and estimate the degree and scale of required interoperability between them: hospitals, pharmacies, billing gateways, labs, health insurers, and more.
- Examine existing communication channels and assess their security to determine corresponding protection strategies (including different and/or combined media like IoT channels, Wi-Fi access points, on-premises wired networking, and more).
- Assess the current state of HL7 standard implementation. Have any HL7 standards previously been adopted and used within the existing healthcare system configuration?
- Map data flows and the messaging scope to be maintained between systems and define the desired level/methodology of system integration.
- Select an HL7 integration strategy. Is it rational to establish point-to-point data exchange between systems, or is it better to set up an HL7 engine instead? (In most cases, modern solutions are engine-based.)
- Select the right model and provider of cloud hosting for the server application supporting data operations and routing. Learn more: Cloud Computing in Healthcare: 3 Use Cases, Benefits, Features & Best Practices.
- Consider all technologies and modules involved, like onsite IoT devices, security systems, EMR, and billing system integrations. They may all require individualized approaches to HL7 implementation for different segments of their networking and connectivity routes.
- Develop a specific concept for how HL7 standards for healthcare information exchange will be applied to cross-system communications using the HL7 Reference Information Model (RIM) and other auxiliary documents. This job should be done by an experienced HL7 integrator and/or medical software engineer so no gaps can remain.
- Define local formatting and technical rules to be applied to messages as well as their transmission methods, coding, and decoding processes.
- Define the scope of functionality and the architecture of the required solution, including the HL7 integration engine or interface to manage traffic across medical systems.
Phase #2: Create an Interoperability Solution with HL7 Specifications and Local Requirements
- Divide the process of HL7 integration engine development into manageable technical specifications and tasks.
- Assign tasks to developers and other medical IT specialists that can execute them. Involve an experienced PM or CTO who is ready to lead and supervise the team through all project stages.
- Apply testing methods to make sure HL7 integration is successful. This can be done with the help of professional QAs with a grasp of HL7 standard specifications and project objectives.
- Consider hiring TATEEDA GLOBAL as your HL7 integration partner for team augmentation services and consulting. ➡️ Learn more about our IT services and hourly rates ⇒
Phase #3: Validate and Maintain Consistency of Your HL7 Integration Results
- Validate the applied HL7 integration method and the efficiency of the HL7 engine/interface built by the team.
- Make sure all outbound messages are transformed into a format that can be accepted by the target system, correctly routed to the endpoint, and accurately processed by the target system(s) for intake.
- Make sure to cover all problems and bugs found while testing HL7 communications, formatting, and interoperability between healthcare systems; iterate until optimal results are achieved.
- Establish a regular routine for HL7 integration process monitoring and medical software maintenance services.
The HL7 Integration Services TATEEDA GLOBAL Offers
With TATEEDA GLOBAL, you can hire experienced IT professionals for your HL7 integration project(s).
- We offer a wide spectrum of medical software development services and can assist you with HL7 standard implementation.
- We develop custom HL7 interfaces that support a variety of HL7 protocols and versions: HL7 FHIR, HL7 v2.x, v3.x, and more.
- TATEEDA helps you with the selection of your HL7 integration platform plus easy-to-use data mapping tools for XML and other standards.
- We have custom interfaces and DevOps for processing complex business logic.
Frequently Asked Questions
Why is HL7 difficult to integrate?
This process requires serious healthcare software development skills and deep knowledge of the standard. There is a limited availability of HL7 integration professionals out there.
What is an HL7 interface engine?
An HL7 interface engine is a central software hub that acquires medical system messages, then parses, filters, transforms, and directs them to target systems. Building an interface engine for HL7 operations is never a one-size-fits-all approach, so this requires deliberate research and customization efforts.
Who uses the HL7 integration software engine?
American and international medical institutions, hospitals, medical centers, clinics, and other healthcare process stakeholders and actors.
Can UX design help improve HL7 compliance?
UX design is not directly related to HL7 compliance or other interoperability matters; however, if a healthcare company requires a complex approach that encompasses UI/UX design and implementation of software with unique dashboards, panels, and interfaces, TATEEDA GLOBAL has UI designers and skilled web solution developers who can help you with that!
Does TATEEDA GLOBAL provide HL7 integration services?
Yes! We would be happy to consider complex medical application projects with HL7 integration and other interoperability management services. If you have specific ideas and requirements, please contact us to discuss the details and receive free consulting!









![Best AI Development Companies [USA] Title Image](https://tateeda.com/wp-content/uploads/2025/11/Best-AI-Development-Companies-for-the-United-States-1-2.jpg)
