How to Integrate Your EHR System with Cerner or Epic Using APIs: A Detailed Guide

This guide provides a structured roadmap for developers, IT managers, and digital health system integrators tackling Epic EHR integration with existing infrastructures. It ensures Epic systems integration enhances clinical workflow efficiency, patient data accuracy, and overall digital health system security.
This guide also explores Epic and Cerner integration strategies designed to…
- Optimize clinical data exchange and interoperability in medical settings.
- Introduce advanced APIs, HL7, FHIR, RESTful protocols, and middleware.
- Reconfigure clinical processes, unlock granular data insights, and construct an unyielding conduit for continuous medical information flow.
Electronic Health Records (EHRs) form the backbone of modern healthcare trends and technologies. They empower clinicians to retrieve, update, and disseminate patient data in real time (a recent AHA study reported that over 95% of U.S. hospitals now utilize some type of EHR/EMR systems).
In the clinical IT environment, safe and organic data exchange across disparate systems and devices is an operational imperative; this dynamic interplay minimizes administrative errors and accelerates precision-driven analytics, allowing for faster identification of treatment patterns and early disease detection, which leads to improved patient outcomes.
Examples of this approach to custom healthcare solution development include:
- Integrated AI-driven analytics in EHR systems, which can swiftly analyze vast datasets to detect sepsis risk in ICU patients, significantly improving response times.
- Predictive modeling algorithms that identify early signs of chronic disease progression enable physicians to implement preemptive treatment plans and reduce hospitalization rates.
Why is connecting custom EHR systems to larger platforms like Epic and Cerner crucial?
Many healthcare organizations deploy custom EHR or EMR solutions that cater to their unique workflows, such as specialized documentation templates for pediatric care, integrated decision-support tools for oncology, or seamless imaging and lab result integration for radiology departments.
However, establishing connections with dominant platforms such as Epic Healthcare Software, which holds a significant 36% market share of U.S. hospitals, or Oracle Health (formerly Cerner), which maintains a stronghold in acute care with a 21.7% market share, via APIs is essential for medical system data interoperability.
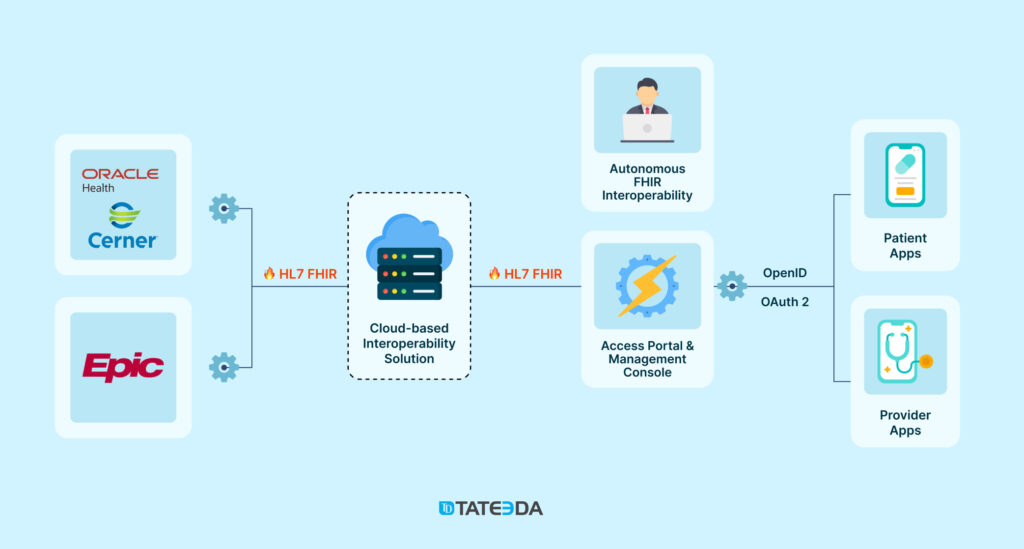
This strategic linkage—often realized through sophisticated integration methods—bridges isolated local systems with expansive healthcare networks, introducing cloud-based FHIR stores to ensure that every fragment of patient data contributes to a cohesive, actionable whole with seamless medical IT system & data interoperability.

Learn more: ➡️ AI Assistant Development Services
What distinguishes Epic and Cerner in the realm of EHR solutions?
Among the digital revolution’s trailblazers, Epic—introduced in 1979 under the leadership of Judith Faulkner—has steadily evolved into a refined system known for its intuitive interface, robust clinical workflow management, and detailed data analytics. These strengths have driven demand for nuanced Epic EHR integration strategies, with many healthcare networks implementing multiple Epic integrations to streamline operations, enhance interoperability, and improve patient outcomes.
Conversely, Cerner, also established in 1979 and now part of Oracle, known as Oracle Health or Oracle Cerner* (the deal was closed in 2022), is renowned for its flexible, interoperability-focused architecture that adeptly manages complex data environments. Institutions favor Cerner integration approaches when they require agile connectivity and meticulous data management across diverse clinical systems, ensuring seamless coordination between healthcare providers and ancillary services. The up-to-date way of referring to Cerner EMR integration in the tech context is calling it Oracle Health integration.
| *Oracle Health has announced plans to introduce a new electronic medical record system, built from the ground up, embedding AI throughout clinical workflows. Set for release in 2025, this next-generation platform was unveiled at the Oracle Health Summit, though its availability outside the U.S. remains unconfirmed. |
What drives the urgent need for API-based EHR integrations?
Local EHR and EMR systems within healthcare organizations (e.g., hospitals, outpatient clinics, long-term care facilities, and specialty practices) are often siloed, limiting their ability to share data with broader networks.
The increasing necessity to connect your EHR system with platforms such as Epic or Cerner via APIs arises from several converging factors:
- Firstly, the imperative for real-time data accuracy (our studies indicate that well-integrated systems can reduce data discrepancies by up to 30%) is critical for informed clinical decision-making;
- Secondly, automating data exchanges substantially reduces the reliance on error-prone manual entries, thereby streamlining operational efficiency;
- Finally, Cerner and Epic integrations unlock the potential for advanced analytics—empowering healthcare organizations to aggregate and mine medical data available to them and engage in predictive modeling and strategic planning with unprecedented precision.

Need Help with Oracle Health or Epic Healthcare Software Integration?
TATEEDA provides a skilled software engineering team to assist with EHR system integration via APIs.
Table of Contents
Making Sense of EHR Integration and API Essentials
Before integrating your local patient data management products (usually locally installed EMRs) with more powerful and global health IT solutions like Epic or Cerner hospital software, you must recognize the risks—technical errors, such as data mismatches, authentication failures, or API response delays, can lead to data loss or misinterpretation.
Nobody wants to face multi-million dollar fines from the government or lawsuits from patients due to compliance failures because of incorrectly configured Cerner or Epic integration! Just imagine if your patients’ critical data, like allergies, were missing from their profiles or outdated. Nurses could administer the wrong medication, leading to severe reactions, legal consequences, and financial liabilities for your organization.
“Getting EHRs to work smoothly with APIs isn’t always straightforward. There are plenty of surprises along the way, but with the right approach and a rigorously selected health tech partner standing by your side, you can avoid major headaches and get Oracle Cerner or Epic EHR integration done efficiently, so no important medical data updates get lost in the shuffle.”
— Andrew G., Senior Software Engineer at TATEEDA
This guide will help you understand and practically apply the key principles of both Epic and Cerner EHR integration with different systems. Let’s consider the technical prerequisites you need to know including the major features of the Epic hospital software and Oracle Health (Cerner):
Electronic Health Record (EHR) systems
EHR systems like Cerner and/or Epic hospital software are centralized platforms that store, manage, and exchange structured patient data across healthcare organizations in the United States. Modern EHR solutions extend far beyond local hospital networks or medical center client bases.
⚡⏩ They enable instant access to nationwide EHR networks through Health Information Exchanges (HIEs), FHIR-formatted cloud interoperability, and federal/state health data frameworks like CommonWell Health Alliance and Carequality, which is the main point of Oracle Health integration, Cerner EMR integration, and Epic systems integration or any other project of this type.
These networks allow medical providers to query and retrieve up-to-date patient records from shared data pools via Cerner and Epic systems integrations, ensuring clinicians always have the most recent and accurate health information at their fingertips. In addition to Oracle Health (Cerner) and Epic, the leading vendors in the U.S. include Meditech, Allscripts, NextGen Healthcare, eClinicalWorks, athenahealth, Greenway Health, Practice Fusion, CareCloud, and DrChrono.

Application Programming Interfaces (APIs)
These are software intermediaries that facilitate secure, standardized communication between EHRs and other healthcare applications. APIs empower health software developers to seamlessly integrate third-party applications, including custom telemedicine platforms, custom patient portal solutions, and custom healthcare billing systems.
Acting as intermediaries, APIs enable structured requests and responses between systems, ensuring that data is exchanged in a standardized and secure manner through Cerner or Epic systems integration. For example, when a hospital’s integrated EHR software requests lab results from an external diagnostic center, an API facilitates this request by securely retrieving and delivering the relevant data to Laboratory Information Management Systems (LIMS), Health Information Exchanges (HIEs), Vendor-Neutral Archives (VNAs), and Clinical Data Repositories to ensure clinicians have immediate access to essential patient information.
They enable continuous data synchronization between multiple systems/databases and automate intricate clinical workflows, covering the entire patient journey—from the initial event in the patient appointment scheduling system and medical record updates to secure healthcare payment software integrations and post-treatment follow-ups. They apply protocols like FHIR (Fast Healthcare Interoperability Resources) and HL7 V2 & V3 to ensure interoperability between hospitals, labs, pharmacies, and insurance systems.
“FHIR breaks down healthcare data into structured packages—this could be patient records, lab results, medication lists—you name it. APIs step in to fetch, share, and update this information instantly. RESTful APIs, built on standard HTTP methods like GET and POST, provide a web-friendly way to make FHIR-based interoperability work smoothly across EHRs, labs, pharmacies, and insurers. No more data silos—just a seamless, two-way exchange between hospitals, mobile health apps, and patient portals.”
— Slava K., CEO of TATEEDA
Regulatory bodies like the ONC mandate FHIR-based APIs for secure, structured patient data access and compliance. By integrating FHIR APIs, healthcare organizations achieve scalable, real-time interoperability that enhances workflow automation, data governance, and patient outcomes.
FHIR vs. HL7 V2 & V3: Understanding Interoperability Standards
| Protocol | Primary Use Case | Key Benefits | Relation to APIs |
| FHIR (Fast Healthcare Interoperability Resources) | Modern, web-based data exchanges | Ideal for cloud interoperability, mobile health apps, and real-time patient data retrieval | Designed for API-driven interoperability, enabling seamless integration between systems through RESTful APIs |
| HL7 V2 & V3 | System-to-system interoperability in legacy environments | Ensures data exchange between traditional healthcare IT systems, widely adopted for hospital data flows | Used in older systems where data exchange follows predefined message formats, often requiring middleware to bridge modern API-based architectures |

Integration with EHR platforms like Cerner and Epic
Integration with industry-leading patient data platforms like Cerner and Epic hospital software ensures seamless data exchange across hospitals, clinics, and specialty care centers. By connecting local EMR/EHR systems to these larger networks, healthcare organizations…
- Enable basic interoperability and compatibility
- Enhance collaboration between medical service providers
- Facilitate more accurate and timely decision-making.
| Without such integrated EHR software, patient data remains isolated, increasing the risk of medical errors, miscommunication, and workflow inefficiencies including manual data entry by administrative staff, doctors, and nurses. This fragmentation hinders the ability of clinicians to access comprehensive patient histories, which can lead to redundant testing, delayed diagnoses, and inefficient treatment plans. |
?? A thoughtfully executed Epic integrations approach ensures that data streams remain coherent across multiple platforms, while a dedicated Cerner integration strategy preserves data integrity. This automation not only diminishes administrative burdens but also supports dynamic, high-pressure clinical environments where timely information is paramount. It makes sure that vital health information is always accessible when and where it is needed—the key benefits include:
- Data Consolidation: Aggregating data from various sources such as laboratory results, imaging systems, pharmacy records, and primary care notes into a single, structured repository. For example, integrating a radiology information system (RIS) ensures that imaging results are instantly available alongside a patient’s medical history, preventing delays in diagnosis.
- Real-Time Access: Providing instant access to patient records, allowing physicians and nurses to retrieve and update data at the point of care. For instance, in emergency rooms, real-time integrated EHR software access can help medical teams make quick, life-saving decisions by instantly reviewing allergy histories and previous treatments.
- Regulatory Compliance: Ensuring adherence to healthcare laws such as HIPAA software validity, GDPR, and CCPA through robust encryption, audit logs, and access controls. Compliance-driven EHRs also integrate Role-Based Access Control (RBAC) and Single Sign-On (SSO) to ensure secure access to sensitive patient data.
- Operational Efficiency: Reducing redundant data entry, automating clinical workflows, and eliminating manual paperwork. For example, automated electronic prescription management in EHRs reduces the risk of medication errors and streamlines pharmacy coordination by directly sending electronic prescriptions to dispensing systems through e-Prescribing and Computerized Physician Order Entry (CPOE).
In clinical environments where every millisecond counts, robust Epic integration as well as correct Cerner EHR integration ensures that all patient data remains unified, uncompromised, and accessible while maintaining data normalization, patient matching, and clinical workflow automation for improved accuracy in every medical process.
Thanks to the interoperability enabled by system components like RESTful APIs, SOAP APIs, and OAuth 2.0 for secure authentication, healthcare providers, administrators, and patients experience effortless connectivity across a wide array of healthcare platforms—from cloud-based Health Information Exchanges (HIEs) and Hospital Information Systems (HIS) to Patient Engagement Platforms and Clinical Decision Support (CDS) tools.

Custom Hospital Software Integration Services
Since 2013, TATEEDA has been delivering software integration solutions. We help you ensure efficient EHR connectivity through API integration.
Pre-Integration Considerations and Prerequisites
Define Your Epic or Cerner EHR Integration Goals
A poorly planned EHR integration can cause more problems than it solves—imagine trying to connect two hospital systems and realizing halfway through that they don’t even recognize the same patient ID format. As far as digital health solutions are complicated, you must carefully align your Epic EHR integration or Cerner integration with existing hospital information systems (HIS) to achieve full interoperability at scale.
- Data Types: Identify what patient data needs to be exchanged—demographics, lab results, prescriptions, and scheduling details are key considerations. Structuring this data using FHIR and HL7 V2/V3 keeps communication standardized across platforms. Proper medical data standardization ensures consistency across all care settings and reduces integration errors.
- Workflow Adjustments: Data integration must complement daily clinical operations instead of disrupting them. Any modifications should enhance computerized physician order entry (CPOE), electronic prescribing (e-Prescribing), and clinical decision support (CDS) rather than create inefficiencies. A focus on clinical workflow optimization can help prevent unnecessary roadblocks.
- Use Cases: Identify real-world applications, such as real-time patient record updates, automated appointment scheduling, or immediate lab result retrieval. Implementing predictive analytics in medicine alongside EHR integration can also support proactive care strategies by identifying risk factors before they escalate into serious conditions.
A well-defined strategy ensures that Epic EHR integration and Cerner EMR integration enhance efficiency, improve patient care, and prevent operational slowdowns.
Ensuring Compliance in Your Cerner & Epic Integration Process
Regulatory compliance in healthcare IT is not an afterthought—it is the foundation that keeps patient data protected and organizations legally secure. Failure to comply with industry standards can result in legal action, financial penalties, and reputational damage. The following steps ensure that Epic EHR integration and Cerner integration meet compliance requirements:
- Implement HIPAA-compliant security measures when working on Epic EHR integration or Cerner EMR integration. Compliance with HIPAA, GDPR (where applicable), and other regulatory frameworks is mandatory. Using RBAC and audit logging ensures that only authorized personnel have access to sensitive patient data while maintaining an accurate record of all access activities.
- Prevent duplicate PHI exposure by establishing structured data deduplication processes. This mitigates security risks while improving the accuracy of population health management initiatives, which depend on comprehensive and error-free datasets.
- Define clear vendor contracts and data-sharing agreements with Cerner integration or Epic EHR integration providers. These agreements should specify data ownership, security measures, and compliance with frameworks such as CommonWell Health Alliance and Carequality to ensure proper interdisciplinary care coordination across different healthcare entities.
Planning for custom-integrated EHR software’s compliance in the early stages of integration prevents setbacks, ensures smooth approvals from regulatory bodies, and strengthens trust between healthcare providers, vendors, and patients.

Technical Prerequisites for a Robust Cerner/Epic EHR Integration
A well-prepared technical environment minimizes failures and bottlenecks, allowing Epic EHR integration and Cerner integration to function efficiently while supporting cloud-based EHR systems for scalability. The following table outlines the critical components required before integration begins:
| Requirement | Purpose | Implementation |
| API Keys & Credentials | Authenticate access to Epic and Cerner systems securely. | Obtain credentials via Epic’s App Orchard or Cerner Open Developer Experience. |
| Sandbox Environment | Provides a controlled space for testing API connections and data flow without affecting live systems. | Request sandbox access through the vendor’s developer portal. |
| Integration Engine | Routes and manages HL7/FHIR messages between systems to maintain structured interoperability. | Use solutions like Mirth Connect or Rhapsody for message processing. |
| Middleware Implementation | Serves as an intermediary layer, allowing legacy systems to interact with modern APIs. | Implement SOA (Service-Oriented Architecture) or microservices-based middleware. |
| Authentication & Security | Ensures encrypted, verified API connections and user identity management. | Utilize OAuth 2.0, Single Sign-On (SSO), and JSON Web Tokens (JWT). |
| Cloud & Containerization | Provides a scalable and consistent environment for deployment and system reliability. | Deploy applications via Docker and Kubernetes. |
| Artificial Intelligence in Healthcare | Enhances data-driven decision-making and predictive analytics. | Implement AI models to analyze clinical trends and support diagnostics. |
| Cybersecurity in Healthcare | Protects EHR systems from breaches, unauthorized access, and data theft. | Apply encryption, endpoint security, and continuous monitoring tools. |
Accessing Developer Resources and Setting Up Your API Integration Environment
Cerner or Epic EHR integration isn’t just about API calls. Precision, security, and compliance define success. For successful Epic or Cerner EHR integration, set up a robust development environment, involve native vendor resources, and enforce best practices—the difference between a flawless rollout and a deployment nightmare.
Cerner and Epic Developer Resources
Buried deep in the archives of EHR vendors lies an ocean of documentation. It’s overwhelming. Necessary? Absolutely. Rather than assembling the puzzle piece by piece, tap into established resources that streamline Epic integration and/or Cerner EHR integration. Consider these must-have starting points:
- Oracle Health Developer Program—a one-stop hub of API documentation, sandbox environments, and prebuilt sample code, connecting local EHRs to Oracle Health’s vast ecosystem.
- Epic App Orchard—a marketplace stacked with API endpoints, integration guides, and technical best practices for embedding custom solutions into Epic’s architecture.
- Regularly updated technical references covering FHIR-based API endpoints, authentication protocols (OAuth 2.0, JWT), data formats (JSON, XML), and compliance frameworks to meet security and interoperability requirements.
API versions evolve faster than a triage unit during peak hours. Staying current isn’t optional—it’s the only way to avoid compatibility issues, regulatory headaches, and system inefficiencies.
Setting Up Your Development Environment
This isn’t just setting up a workspace—it’s preparing the foundation for seamless Cerner integration and Epic EHR integration. Every decision made at this stage affects data exchange, system performance, and debugging agility. Here’s how to get it right:
- Choose an IDE: Visual Studio Code or PyCharm provide debugging support, API testing plugins, and terminal access—core essentials for healthcare integrations.
- Set Up API Clients: Tools like Postman or Insomnia enable structured endpoint validation, authentication testing, and real-world data exchange simulations.
- Implement Version Control: GitHub or GitLab keep track of code history, collaboration efforts, and rollback capabilities when something (inevitably) needs fixing.
- Select Programming Languages: Python, Java, or Node.js—each optimized for FHIR interoperability, JSON parsing, and handling high-volume API requests.
- Adopt Suitable Frameworks: Flask/Django (Python), Spring Boot (Java), or Express.js (Node.js) streamline API request management, security implementations, and system communication.
- Configure Testing Environments: A sandbox should be an exact replica of production settings, covering authentication, rate limits, and structured test data models.
- Integrate Continuous Deployment: Automation tools like Jenkins, GitHub Actions, or GitLab CI/CD handle security scans, regression testing, and zero-downtime deployments.
Establishing a Secure Environment
| Component | Purpose | Tools/Examples |
| API Keys & Credentials | Restrict unauthorized access and authenticate API requests. | Obtain from Epic’s App Orchard or Oracle Health Developer Program. |
| Sandbox Environment | Simulate real-world API behavior and validate system integrations. | Access via vendor-specific developer portals. |
| Authentication & Security | Encrypt transmissions, verify identities, and enforce HIPAA compliance. | Implement OAuth 2.0, Single Sign-On (SSO), and JSON Web Tokens (JWT). |
| Cloud & Containerization | Scale, deploy, and maintain infrastructure consistency. | Use Docker and Kubernetes for seamless cloud deployment. |
Cerner or Epic EHR Integration Workflow and Best Practices
A well-planned Epic system integration or Cerner EHR integration isn’t just about pushing code—it’s about ensuring long-term stability, security, and regulatory compliance. The key to success? Rigorous testing, airtight security, and a deployment strategy that prioritizes resilience over speed.
Authentication and Authorization with OAuth 2.0
Both Cerner and Epic rely on OAuth 2.0 as the foundation of secure authentication and authorization, ensuring that every data exchange meets strict security standards.
The process begins with registering your application with the EHR vendor, granting a Client ID and Client Secret—credentials essential for establishing system trust. Once registered, users must be directed to the vendor’s authorization endpoint, where they explicitly grant access to the integration.
After approval, the received authorization code must be exchanged for an access token (and, if applicable, a refresh token) via a POST request to the token endpoint. This access token serves as a secure key, enabling real-time retrieval of protected patient data while maintaining strict authentication and authorization controls.
Managing these tokens properly is critical—secure storage, timely refreshes, and proper handling of HTTP methods (GET, POST, PUT, DELETE) ensure system integrity, regulatory compliance, and prevent unauthorized access.
Connecting to API Endpoints: A Step-by-Step Process
Once authentication is firmly in place, the next step is to establish a connection with the EHR’s API endpoints. This structured workflow ensures seamless Cerner EHR integration and Epic hospital software integration:
- Establish a Connection – Initiate communication by sending a simple GET request (for instance, to a /metadata or /system/status endpoint) using a tool like Postman to verify connectivity.
- Retrieve Data – Query patient demographics, clinical data, or appointment schedules from FHIR endpoints (e.g., /Patient, /Observation) to ensure structured information is accessible and correctly formatted.
- Post or Update Data – Use POST requests to create new records or PUT/PATCH requests to modify existing records, ensuring that payloads conform precisely to the required FHIR resource structure.
- Implement Data Synchronization – Apply mapping and transformation logic to align local EHR data with that of Cerner or Epic, ensuring consistent and harmonized records across systems.
- Handle API Responses – Monitor HTTP status codes and error messages (e.g., 200 OK, 400 Bad Request, 500 Server Error) to diagnose issues promptly. Robust error-handling routines are vital for troubleshooting and maintaining system stability.
A structured API connection process ensures that every data exchange is executed with precision, enhancing interoperability between disparate systems.
Data Mapping, Transformation, and Handling
Interoperability demands that data from diverse sources be transformed into a consistent, standardized format. Meticulous data mapping is key to ensuring accurate and meaningful exchanges across healthcare systems. Follow these steps to guarantee a seamless data transformation process:
- Identify Key Data Fields – Extract essential patient identifiers such as names, dates of birth, medical record numbers, and treatment history from your local EHR system. Ensure that fields align with standardized patient information models to prevent mismatches when integrating data from multiple sources.
- Map Data to FHIR Resources – Align extracted data with FHIR-compliant structures, ensuring that fields match predefined industry standards (e.g., mapping patient IDs to Patient.identifier). Common resources include Patient, Encounter, Observation, Condition, and MedicationRequest.
- Develop Transformation Logic – Use middleware, ETL pipelines, or custom scripts to convert native EHR data formats into FHIR-compliant JSON or XML representations. Ensure that all numeric values, timestamps, and coded elements conform to HL7 and FHIR standards.
- Validate Against FHIR Schemas – Cross-check transformed data using FHIR validation tools or schema checkers to confirm compliance with industry standards. Tools like HL7 Validator, Inferno, or HAPI FHIR can automate this validation.
- Implement Data Synchronization – Set up real-time or scheduled synchronization processes between Epic, Cerner, and other healthcare networks, ensuring data integrity and consistency. Use FHIR Subscriptions, message queues, or API polling mechanisms to maintain up-to-date records across systems.
“In practice, whether Cerner integration or Epic EHR integration goes beyond just being functional—they must be precise, secure, and fully interoperable. Ensuring patient data is available when and where it’s needed requires robust validation at every step. From synchronizing medical histories to retrieving lab results and streamlining system-wide communication, every integration must be both efficient and reliable.
Based on our experience, this approach generally delivers strong results, but no two clients are the same. Each integration must be tailored to account for infrastructure differences, compliance obligations, and workflow nuances to achieve optimal performance.”— Anastasia M., Team Tech Lead at TATEEDA
Testing and Debugging Your Integration
A flawless Epic EHR integration or Cerner EHR integration doesn’t happen by chance—it’s the result of rigorous testing and continuous debugging. Every API call, every data transformation, and every workflow must be validated under real-world conditions. Skipping this phase? That’s a surefire way to invite system failures, compliance violations, and unpredictable user experiences. A structured, systematic approach ensures issues are caught early and resolved before they spiral into full-scale disruptions.
Step-by-Step Cerner or Epic Integrations Testing Process
| Step | Action | Tools/Examples |
| 1. Sandbox Deployment | Run integration tests in an isolated, non-production environment identical to the live system. | Vendor-provided sandbox environments (Epic, Oracle Health). |
| 2. Unit Testing | Validate API requests, responses, and data transformation accuracy at the lowest level. | pytest (Python), JUnit (Java), Mocha (Node.js). |
| 3. Integration Testing | Simulate end-to-end workflows across interconnected EHR systems, verifying data consistency. | Postman, Newman, Cypress. |
| 4. Error Simulation | Intentionally introduce incorrect credentials, missing fields, or network failures to evaluate system resilience. | Fault injection frameworks, Chaos Monkey. |
| 5. HTTP Response Monitoring | Analyze response times, status codes (200 OK, 400 Bad Request, 500 Server Error), and error logs. | Splunk, ELK Stack, Datadog. |
Security, Compliance, and Data Privacy
EHR integration isn’t just about connecting systems—it’s about safeguarding patient data while ensuring compliance with strict regulatory requirements. Every API call transmits sensitive healthcare information, demanding encryption, controlled access, and continuous monitoring. Epic EHR integration and Cerner integration require robust security protocols that guard against unauthorized access, data breaches, and compliance violations.
Step-by-Step Security Protocol
| Component | Purpose | Implementation Example |
| Encryption (TLS/SSL) | Encrypts data in transit, ensuring secure API communication and preventing unauthorized interception. | Enable TLS 1.2+ on all API endpoints and enforce HTTPS-only traffic. |
| Role-Based Access Control (RBAC) | Restricts access to patient data based on user roles and organizational policies. | Implement OAuth 2.0 scopes, integrate with Okta, Azure AD for identity management. |
| Secure Data Storage | Protects patient data at rest using advanced encryption and integrity controls. | AES-256 encryption, database tokenization, and access logging. |
| Regulatory Adherence | Ensures compliance with HIPAA, GDPR, and ONC certification for legal and ethical patient data handling. | Conduct periodic third-party compliance audits, enforce data retention policies. |
| Audit Logging & Monitoring | Tracks API usage, logs access attempts, and flags suspicious activity in real time. | SIEM solutions (Splunk, ELK Stack, AWS CloudTrail). |
Deployment, Monitoring, and Maintenance
Going live is just the beginning. A well-executed deployment strategy ensures that EHR integrations remain stable, performant, and secure. Controlled rollouts, proactive monitoring, and disaster recovery mechanisms keep everything running smoothly. Every second of downtime in healthcare matters, so staying ahead of failures is mission-critical.
Step-by-Step Deployment Process
| Step | Action | Tools/Examples |
| 1. Staged Rollout | Deploy the integration in controlled phases, starting with a small user segment before full-scale release. | Blue-green deployments, A/B testing strategies. |
| 2. Backup & Recovery | Establish failover mechanisms and disaster recovery plans to prevent data loss. | Automated database backups, multi-region cloud replication. |
| 3. Version Control | Maintain a structured repository to manage code changes, rollbacks, and continuous improvements. | Git, GitHub, GitLab CI/CD pipelines. |
| 4. Performance Monitoring | Track API latency, request success rates, and system throughput to maintain real-time responsiveness. | Prometheus, Grafana, AWS CloudWatch. |
| 5. Alert Systems | Automate anomaly detection and set up alerts for security breaches or unexpected downtime. | PagerDuty, Datadog, Nagios. |
| 6. Regular Audits | Conduct frequent compliance and security audits to stay aligned with evolving regulations. | HIPAA assessments, internal and third-party audits. |
| 7. Documentation Maintenance | Keep detailed records of integration workflows, API configurations, and troubleshooting protocols. | Confluence, internal wikis, automated documentation tools. |
The Final Word
EHR integration isn’t just about making systems talk to each other; it’s about making sure they speak the same language, at the right time, with absolute security. When things go wrong, they go very wrong—data mismatches, delayed API calls, or even security breaches caused by poorly configured middleware can lead to lost patient records, compliance violations, and open doors for cyber threats.
At TATEEDA, we don’t just connect systems; we build hacker-proof HL7 FHIR interoperability engines that keep your data accurate, your workflows efficient, and your integrations resilient against attacks. Whether you need Cerner or Epic integration partners to install cloud-based components for seamless EHR connectivity or deploy secure Cerner and Epic system integrations, our HIPAA-compliant AWS cloud development services ensure that your healthcare data moves fast, securely, and in full compliance with regulations.
Don’t let faulty integrations put your healthcare operations at risk—TATEEDA helps you do it right, from architecture to deployment, with security and reliability built in from day one.










![Best AI Development Companies [USA] Title Image](https://tateeda.com/wp-content/uploads/2025/11/Best-AI-Development-Companies-for-the-United-States-1-2.jpg)
