Healthcare Staffing Automation Solutions: Fixing Credentialing & Compliance

For decades, verifying credentials in the United States healthcare meant days on phone calls, chasing down faxes, and wrestling with paper files. That manual approach can’t keep pace with today’s urgent staffing needs, and it drains time better spent on patient care.
In the following sections, we’ll unpack each stage of the credentialing journey, show how custom healthcare software development solutions replace manual steps with automated credentialing services and processes, and explore how these healthcare workforce automation tools can bring clarity and confidence to every phase of provider verification.
Before we drill further into healthcare staffing automation solutions enhanced by automated credentialing services, let’s reaffirm how crucial credentialing is to corporate compliance for healthcare professionals in the U.S.
🩺📋 Credentialing confirms that every nurse, physician, or allied health professional holds the right qualifications, training, and standing. The main components include:
- Confirmation of current, valid professional licenses (verified against state boards and FSMB records)
- Validation of academic degrees and specialized training (primary‐source checks via NCQA-approved processes)
- Verification of board certifications and specialty credentials (through certifying bodies and CAQH ProView)
- Review of employment history and professional references
- Examination of any disciplinary records or sanctions, including federal exclusion lists (OIG–LEIE, SAM) and NPDB queries
- Confirmation of DEA registration for clinicians who prescribe or handle controlled substances
Healthcare workforce automation tools offer a faster, more dependable alternative.
Depending on their role—whether a registered nurse, physician assistant, or surgeon—candidates must assemble state licenses, diploma transcripts, board certificates, proof of malpractice coverage, and signed references.
These records go straight to licensing boards, certifying bodies, the National Practitioner Data Bank, and agencies like CMS. In the U.S., NCQA’s standards and state health departments set the rules, and compliance management software for healthcare helps teams track every requirement and deadline.
Automated credentialing services use secure software links to pull license statuses, training rosters, exclusion lists (OIG–LEIE, SAM), and malpractice reports (NPDB) directly from official databases.
With minimal hands-on work, they connect to CAQH ProView, FSMB’s FCVS, state boards, and federal registries. These platforms meet Joint Commission criteria and HIPAA rules, so they’re fully legal and recognized across the country.
Most credentialing automation platforms provide APIs or modules that plug into custom HR or human-capital systems used by hospitals and clinics. Embedding credential data into onboarding tools and access-management systems keeps a single, up-to-date source of truth. That integration frees administrators from hopping between programs and helps teams stay aligned.
| Verification Element | What It Confirms | Primary Source / Authority |
| State Licensure | Active, unrestricted license in each practice jurisdiction | State licensure boards; FSMB for physician records |
| Academic Degrees & Training | Graduation and completion of residencies or fellowships | Medical/nursing schools; NCQA-approved verification |
| Board Certification | Specialty status and expiration | Certifying boards; CAQH ProView |
| Employment History | Dates of service, gaps, and reasons | Former employers; professional references |
| Disciplinary Records & Sanctions | Malpractice payments, sanctions, exclusions | NPDB; OIG–LEIE; SAM |
| DEA Registration | Authority to prescribe or handle controlled substances | DEA registry |
| CAQH ProView | Centralized provider-submitted credential data | CAQH nonprofit alliance |
| FSMB FCVS | Permanent, primary-source repository of physician credentials | Federation of State Medical Boards |
| NCQA’s Standards | Criteria for what and how often verifications must be performed | National Committee for Quality Assurance |
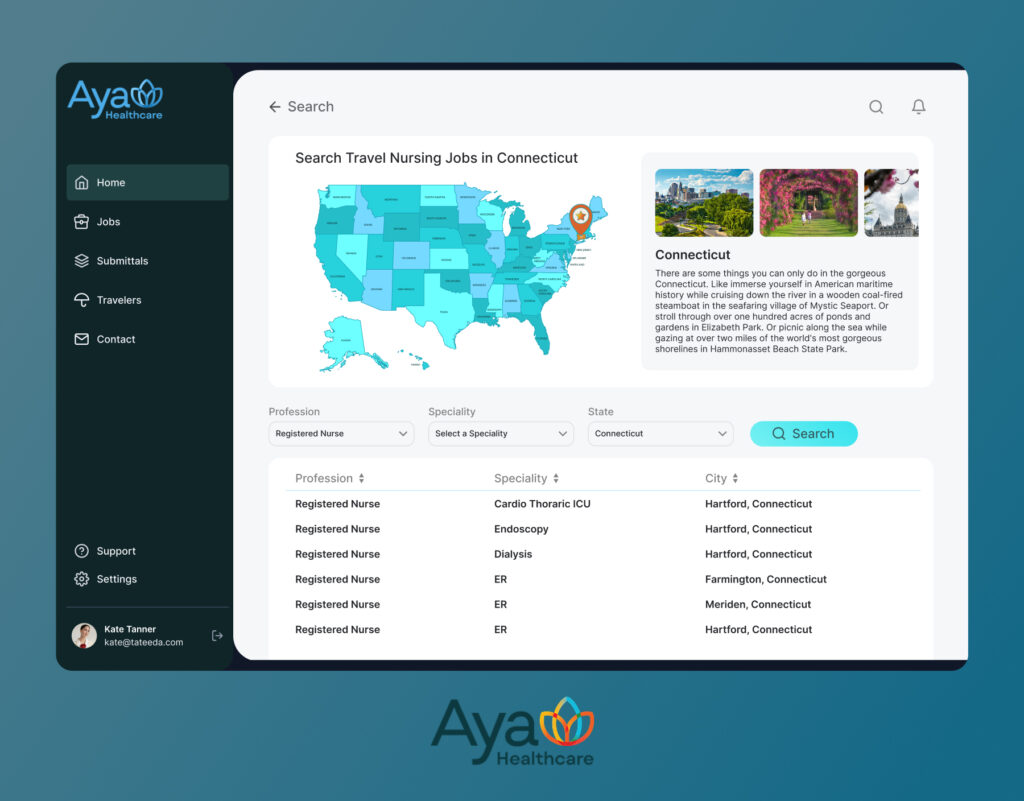
| Why are we qualified to speak about healthcare staff credentialing software? TATEEDA partnered with AYA Healthcare to build a bespoke credentialing automation platform that integrates state board verifications, CAQH ProView feeds, DEA and NPDB checks, and HIPAA-compliant data vaults. Our team of over 100 senior software engineers architected and delivered a solution that cut credentialing cycle times by more than half, all while maintaining full audit trails and regulatory alignment. Drawing on that real-world success and our deep background in compliance management software for healthcare, we know exactly what it takes to design and scale reliable automated credentialing services. |

Embrace the Benefits of Automating Compliance in Healthcare Staffing
Our senior software development team knows how to improve credentialing efficiency with custom HR solutions for healthcare.
Table of Contents
The Top 5 Challenges in Manual Credentialing and How Custom Automation Solutions Solve Them
Managing Timelines and Deadlines
One of the biggest challenges in manual healthcare credentialing is keeping track of multiple expiration dates, payer deadlines, and re-credentialing windows. When reminders live in scattered calendars or sticky notes, it’s all too easy to miss a cutoff and face provider suspension.
Learning how to improve credentialing efficiency starts with a system that treats deadlines as first-class data.
“At one of our partner clinics, a missing license renewal notification sidelined two nurse practitioners for nearly six weeks—patients had to be rescheduled and revenue dipped sharply.”
— Andrew G., Senior Developer at TATEEDA
The following features illustrate how a custom credentialing software solution can resolve this challenge:
- Centralized schedule dashboard with color-coded renewal windows
- Configurable alert engine (email, SMS, in-app)
- Dynamic mapping of payer-specific turnaround times
- Audit log of all deadline notifications and acknowledgments.
Reliance on Manual Processes
Relying on faxes, spreadsheets, and inbox forwards invites errors and delays. Moving from paper to automated credentialing services is at the heart of modern healthcare staffing automation solutions—it means data entry, form validation, and follow-ups happen without human handoffs.
“One client spent 15 hours a week hand-bundle-mailing credential packets. After we introduced a digital form builder and auto-routing, they cut that down to half an hour.”
— Anastasia M., Tech Lead at TATEEDA
Below are the core features your system should include to eliminate manual bottlenecks:
- User-friendly provider portal with guided data entry
- Automatic OCR document upload and field extraction
- Workflow engine for conditional task routing
- Electronic signature and approval tracking.

Learn more: ➡️ Nearshore Software Development Services
Fragmented Data and Missing Documents
When credential files live in silos, it’s nearly impossible to spot a missing diploma or outdated certificate. Healthcare workforce automation tools let you centralize every document, tag metadata, and automate completeness checks, reducing errors in healthcare staff credentialing before they become billing or compliance headaches.
“A hospital realized too late that eight physician files lacked current board certificates. We built a unified repository with completeness indicators, and now every missing item shows up on a single screen.”
— Igor K., Web Technology Architect at TATEEDA
To address fragmentation and ensure no file goes missing, consider these solution components:
- Central document repository with custom metadata fields
- Automated completeness scans and “missing item” alerts
- One-click primary-source verification links
- Full-text search across all credential records.
Security and Compliance Risks
Storing Social Security numbers, licenses, and malpractice histories demands more than locked cabinets—it calls for compliance management software for healthcare that encrypts data, controls access, and proves audit readiness. The benefits of automating compliance in healthcare staffing include airtight logs and consistent enforcement of privacy policies.
“After a minor breach at a staffing agency, we implemented end-to-end encryption and role-based access. A year later, their compliance audit was flawless—no findings.”
— Slava K., SEO at TATEEDA
A robust system should offer the following security and compliance safeguards:
- Encryption at rest and in transit
- Granular, role-based access controls
- Automated exclusion-list screening (OIG, SAM, NPDB)
- Comprehensive audit trail with time-stamped events.
Limited Integration and Scalability
Patchwork integrations force teams to juggle different tools and APIs. Credentialing automation platforms offer modular connectors—whether you need a link to state licensure boards, CAQH ProView, or your custom medical HR management system—to ensure data flows seamlessly and scales as you grow.
“A large multi-site network wanted one view into all provider credentials. We built reusable API modules that now serve nine hospitals and counting.”
— Andrew G., Senior Developer at TATEEDA
Your custom solution can include these integration-focused capabilities:
- Plug-and-play API connectors for boards and registries
- Event-driven microservices for real-time data sync
- Multi-tenant architecture to support dozens of facilities
- SDKs for rapid integration with third-party HR and ERP systems.

Benefits of Automating Compliance in Healthcare Staffing
Faster Onboarding and Reduced Delays
By coordinating concurrent API calls to state boards, DEA, NPDB, and CAQH, a custom platform can be used to show how to improve credentialing efficiency at scale. Multiple verifications—license checks, background screens, and board certifications—run in parallel, overcoming credentialing delays in healthcare that once left clinicians sidelined for weeks.
Event-driven triggers then update each candidate’s status immediately, so coordinators only review exceptions instead of entire applications.
The following features illustrate how a custom credentialing software solution can resolve this challenge:
- Parallel microservices for license, certification, and sanction checks
- Automated expiration alerts tied to configurable deadlines
- Exception dashboards highlighting records needing human review.
Improved Accuracy in Credential Verification
Automated schema validation enforces exact formatting for license numbers, dates, and credential IDs, reducing errors in healthcare staff credentialing caused by manual entry.
Cross-referencing every record against primary-source databases (state boards, NPDB sanctions) catches discrepancies before they reach payers. Immutable audit logs record every change—who made it, when, and why—so you maintain a rock-solid chain of custody.
Key features include:
- Field-level validation rules and checksum verification
- Scheduled cross-database reconciliation reports
- Tamper-evident audit trails with user, timestamp, and change details
- Duplicate-record detection and merge workflows.
Seamless Cross-Department Collaboration
When credential statuses feed directly into HR modules, payroll systems, and shift-planning tools via a unified API, you eliminate hand-offs and email back-and-forth, streamlining healthcare staffing processes across the board.
Role-based dashboards display task ownership, approval history, and document completeness, while webhook notifications keep everyone in sync. This unified approach means your clinical and administrative teams share one source of truth.
Core capabilities include:
- Role-based work queues with task assignment rules
- SSO integration and shared status indicators in staffing schedules
- In-app chat and comment threads on specific credential records
- Calendar hooks to block uncredentialed staff from shift boards
- Mobile push notifications for urgent action items.
Flexible Compliance Controls
A configurable rule engine lets administrators encode licensure requirements, renewal intervals, and exclusion criteria without a single code deployment, offering real-world solutions for healthcare compliance issues. When a state board changes its process or NCQA updates standards, you simply update the parameters in the policy UI, enhancing regulatory adherence through automation. New rules apply immediately to all active profiles.
Essential features include:
- Dynamic rule definitions for DEA, board, and specialty criteria
- Versioned policy library with rollback capability
- “Effective date” enforcement to phase in new requirements
- Automated policy-change notifications to downstream systems.

Strategic Resource Management
Real-time analytics on cycle times, backlog sizes, and error rates empower managers to deploy staff where they’re needed most, delivering clear cost savings with automated credentialing systems. By forecasting credential-renewal peaks and staffing demands, you avoid both overtime expenses and revenue losses from unfilled roles.
Practical features include:
- Dashboard metrics for hours saved per credential cycle
- Predictive modeling of upcoming renewals and workload spikes
- Automated scaling of cloud-based verification services during peaks
- Budget impact reports comparing manual vs. automated processes.
Data-Driven Process Refinement
Rich reporting tools track approval latency, exception counts, and audit scores, demonstrating the impact of automation on healthcare staffing compliance. With automated surveys and ML-driven pattern analysis, you pinpoint remaining bottlenecks and refine workflows iteratively. This continuous feedback loop ensures the system evolves alongside your operational goals.
Valuable features include:
- Custom KPI dashboards for cycle times, error rates, and compliance gaps
- Automated user-experience surveys triggered after credential approval
- Machine-learning alerts for emerging exception patterns
- Heatmaps showing high-volume tasks to guide further automation
- Configuration-driven workflow tweaks without code changes.

Unlock Faster Compliance in Healthcare Staffing
Backed by years of hands-on experience, our senior developers build tailored HR systems that cut credentialing cycles in half and keep every provider up to date.
Essential Healthcare Workforce Automation Tools for Credentialing Solutions
Each of the following modules, powered by healthcare workforce automation tools, creates a cohesive ecosystem where staffing, scheduling, and credentialing operate in concert, delivering a truly modern, efficient, and compliant workforce management platform.
#1. Unified Staff Management Dashboard
A centralized console powered by leading healthcare staffing automation solutions aggregates HR profiles, shift rosters, and credential statuses into a single view.
Administrators immediately spot who is ready to work, who needs missing documents, and which providers are blocked from scheduling due to lapsed credentials.
Scenario: A credentialing lead notices that three PRN nurses on next week’s schedule have pending state license renewals. She reassigns their shifts and triggers automated renewal reminders, eliminating last-minute coverage gaps.
Key Features:
- Role-specific dashboards showing active, pending, and suspended staff
- Real-time calendar overlays of credential expiry dates and planned shifts
- Drill-down panels for comprehensive verification histories
- Automated exception alerts for missing or incomplete files.
#2. Bi-directional API Integrations with Credentialing Providers
By embedding automated credentialing services into your platform, you create live links to CAQH ProView, FSMB FCVS, Nursys e-Notify, state licensure boards, and federal exclusion lists. Whenever a provider updates a profile or a sanction is recorded, your system ingests the change and updates internal records instantly.
Scenario: A surgeon’s board certification posts overnight to the FSMB FCVS feed. At 6 AM, his privileges are auto-updated, and the OR scheduler can assign him to cases without manual sign-off.
Core connectors:
- RESTful APIs and webhooks to push/pull credential data
- Middleware adapters mapping external schemas to internal data models
- Batch reconciliation jobs for conflict resolution.
#3. AI-Driven Document Processing and Validation
Our healthcare workforce automation tools use OCR and machine-learning classifiers to parse diplomas, licenses, and certification cards.
The system extracts fields (names, dates, license numbers) and uses NLP to flag mismatches (e.g., incorrect date formats or name spelling variations). Low-confidence extractions get routed to credentialing specialists for rapid review.
Scenario: A clinician uploads a blurry scan of her nursing diploma at midnight. By 8 AM, the system has extracted her graduation date, compared it against National Student Clearinghouse records, and marked the file as “verified” without human intervention.
Technical Components:
- State-specific OCR templates covering all 50 boards
- Confidence scoring to prioritize manual checks
- Automatic redaction of sensitive fields (SSN, bank details)
- Integration with a custom healthcare AI agent solution
- Integration hooks for human-in-the-loop review.
#4. Automated License Expiry Tracking and Renewal Workflows
Leveraging compliance management software for healthcare, you configure rules that monitor every credential date like licensure, DEA, board certifications, and generate renewal tasks well before expiration.
Multi-stage reminder campaigns (180, 90, 30 days before) can be sent via email, SMS, or in-app notification. Providers follow embedded links to pre-populated renewal forms, dramatically cutting turnaround.
Scenario: An NP receives an SMS 120 days before her DEA expires, taps a secure link to pay renewal fees, uploads her receipt, and closes the loop—all on her smartphone in under five minutes.
Workflow Features:
- Configurable reminder schedules with escalating notification channels
- Pre-filled renewal forms injected into state board portals
- Automatic status blocking for expired credentials
- Dashboards tracking renewal completion rates
- Historical logs for audit and reporting.

#5. Role-Based Access and Immutable Audit Trails
Grant precise permissions so HR clerks, credentialing specialists, clinical leads, and auditors see only relevant data. Every action, whether approving a background check or editing a license number, is recorded in an append-only audit stream. Tamper-evident logs ensure you meet Joint Commission and state survey requirements without manual report assembly.
Scenario: During a surprise NCQA audit, the compliance officer exports a timestamped audit report that shows exactly when each physician’s NPDB query passed and who signed off, satisfying surveyors in minutes.
Security Measures:
- Fine-grained ACLs for view, edit, and approve rights
- Append-only audit logs with cryptographic checksums
- On-demand audit report generation.
#6. Scheduling Integration with Eligibility Enforcement
By linking credential statuses to the scheduling engine, your system automatically prevents uncredentialed staff from appearing on the roster.
Eligibility rules, e.g., “only RNs with current BLS certifications may be assigned to med-surg shifts”, are enforced in real time. Managers see immediate feedback when building schedules, and override requests generate an audit trail.
Scenario: A nurse manager attempts to schedule a new hire for an ICU shift, but the platform blocks the assignment because the BLS upload was still under AI-driven validation. The manager uses the portal’s chat widget to notify the new hire directly.
Scheduling Controls:
- Conditional shift-assignment rules based on credential tags
- Real-time roster validation and blocking alerts
- Manager override workflows with timestamps and reasons
- Calendar hooks to reflect eligibility changes immediately.
# 7. Predictive Compliance Analytics
Using historical data on renewal lead times, exception rates, and document turnaround, machine-learning models forecast upcoming credentialing bottlenecks. Dashboards surface which provider cohorts (e.g., locum tenens, travel nurses) will need extra support, allowing you to scale resources proactively and avoid manual backlogs.
Scenario: Analytics predict a 40% spike in re-credentialing tasks next quarter due to batch expirations. The credentialing manager pre-allocates two contract specialists and avoids a weeks-long backlog.
Analytics Tools:
- Time-series forecasting of expiration peaks
- Anomaly detection for extended verification cases
- Scenario simulations for staffing plans
- Drill-down views by department, location, or role
- Automated alerts are sent when forecasted workloads exceed thresholds.
8. Mobile Self-Service Portal with Contextual Notifications
Providers use a native app or a responsive web portal to upload documents, view credential status, and initiate renewals anytime, anywhere.
Contextual notifications, like a prompt to complete fingerprinting or re-attestation, arrive via push or SMS, with direct links to the exact task. Two-way messaging keeps lines open between providers and their credentialing teams.
Scenario: A doc traveling between hospitals receives a push notification that her state license renewal is due in 30 days. She snaps a photo of her new license, uploads it, and the system confirms acceptance before her next shift.
Portal Features:
- Push notifications tied to specific tasks and deadlines
- In-app guidance linking to required forms and URLs
- Two-way messaging with credentialing specialists.
Integrating Clinical Systems and EMR/EHR for Credentialing and Beyond
Real-Time User Provisioning and Access Control
With modern healthcare staffing automation solutions, as soon as a provider’s license clears verification, the platform automatically provisions EHR accounts, granting access to Epic, Cerner, or Athenahealth, while ensuring deprovisioning if a credential lapses. This eliminates hours spent on IT ticket queues and prevents orphaned logins that pose security risks.
“When we integrated Epic’s user management API for a major nurse agency, providers’ EHR roles updated within minutes of a license change. This eliminated orphaned accounts and boosted security compliance, which the team greatly appreciated.”
— Slava K., SEO at TATEEDA
Automated Primary-Source Verification
To eliminate manual phone calls and faxed documents, automated credentialing services connect directly to CAQH ProView, FSMB FCVS, Nursys e-Notify, and state board APIs. New entries or updates in those primary sources flow into your HR/EHR system in minutes, replacing days-long verification cycles with instantaneous, auditable checks.
“For a regional clinic, we built a REST connector to CAQH ProView that processed overnight updates for over 100 clinicians. This cut manual verification effort by 80% and earned high praise from the credentialing staff.”
— Andrew G., Senior Developer at TATEEDA
Unified Compliance Dashboards
Compliance management software for healthcare consolidates audit logs, sanction screenings (OIG LEIE, SAM, NPDB), and policy updates into a single pane of glass. Survey-ready reports, broken down by department or facility, can be generated on demand to demonstrate credential status, renewal histories, and exception resolutions without manual data gathering.
Shift Assignment Safeguards
By leveraging healthcare workforce automation tools, your scheduling engine can enforce eligibility rules such as “only RNs with current BLS and ACLS may staff ICU shifts” at the moment you build a roster. Any violation triggers a clear alert, blocking the assignment and notifying both the manager and clinician of missing requirements.
Scalable Workflow Orchestration
Our healthcare staffing automation solutions rely on credentialing automation platforms to orchestrate microservices such as OCR, license expiry monitoring, renewal workflows, and primary-source queries across a multi-tenant cloud environment. This architecture scales seamlessly as you add new facilities or provider types, ensuring consistent performance and compliance at every level.
The Final Word: How TATEEDA Helps You Create Healthcare Staffing Automation Solutions
As a trusted partner to one of the largest travel nurse agencies in the United States, TATEEDA has brought together HR platforms, scheduling engines, and credentialing modules into a single, cohesive system.
Our custom healthcare software integration services focus on overcoming credentialing delays in healthcare staffing by automating license checks, CAQH feeds, and sanction screenings so clinicians can hit the floor without needless hold-ups.
We also enhance regulatory adherence through automation, building audit-ready workflows that capture every verification step and permission change. The result is clear cost savings with automated credentialing systems, less time spent chasing paperwork, and more resources directed to patient care!

Are You Ready for Healthcare Staffing Automation Solutions?
Let TATEEDA help you unite staffing, compliance, and clinical access into one seamless solution.









![Best AI Development Companies [USA] Title Image](https://tateeda.com/wp-content/uploads/2025/11/Best-AI-Development-Companies-for-the-United-States-1-2.jpg)
